Interns are not (yet) poisoned by the STEMI/NSTEMI paradigm
Dr. Smith's ECG Blog
JUNE 10, 2025
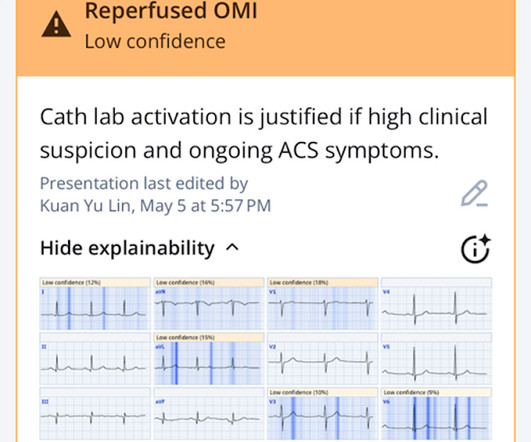
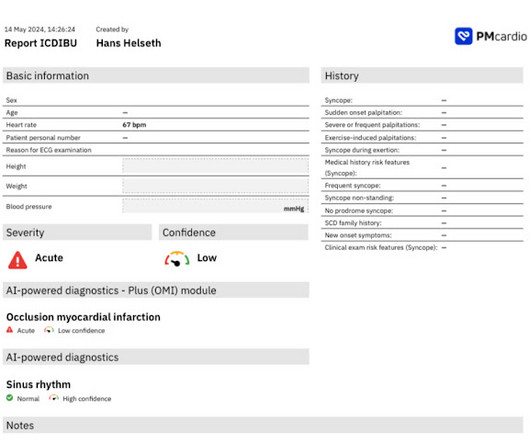
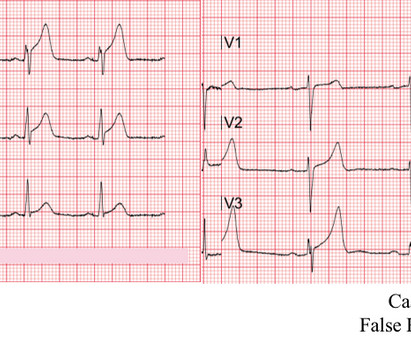
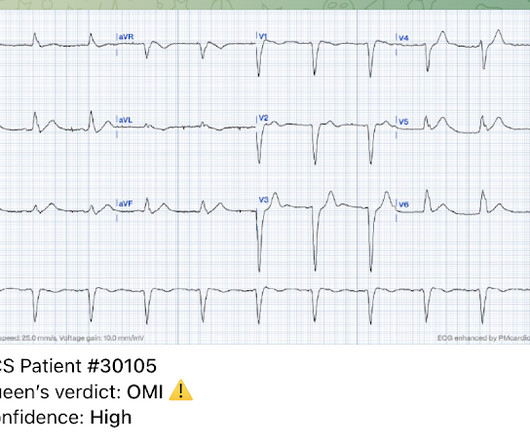
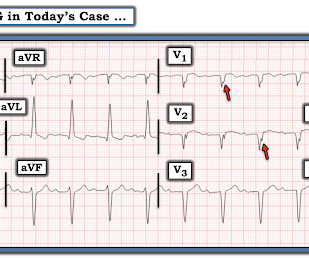
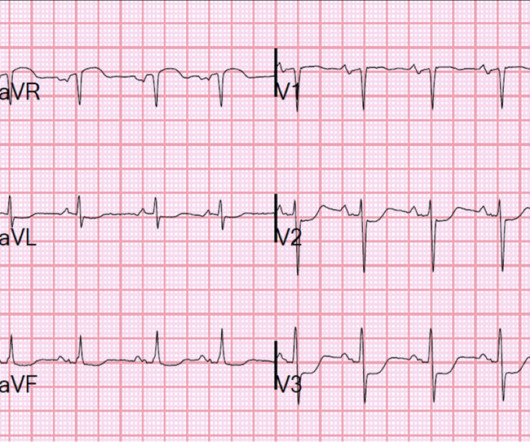
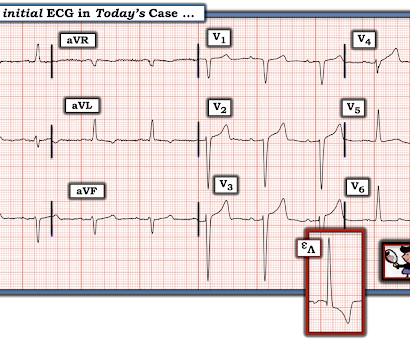
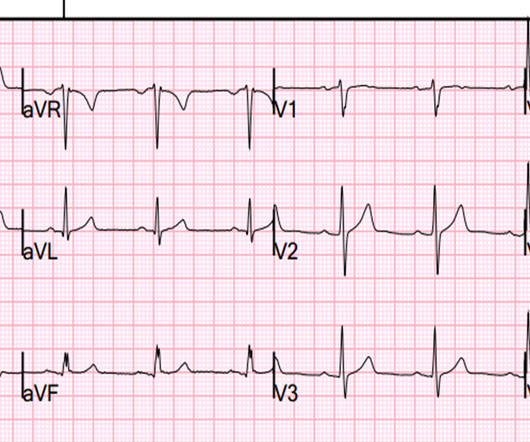
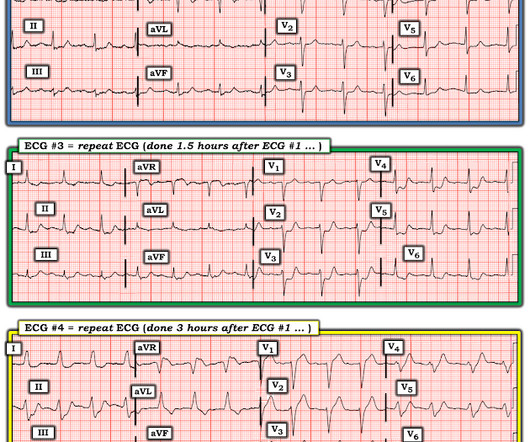
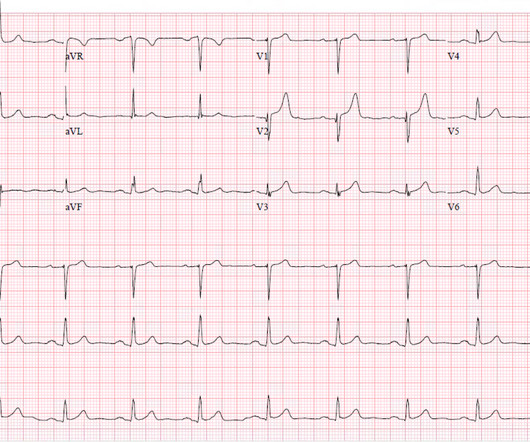
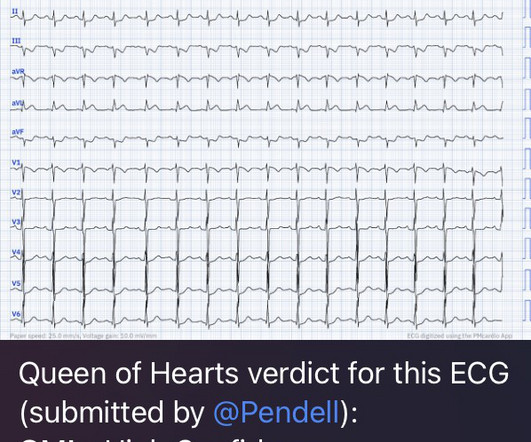
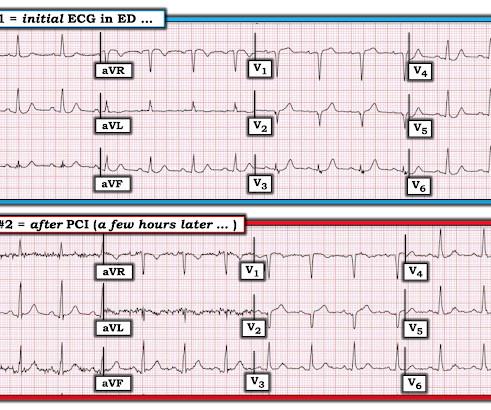
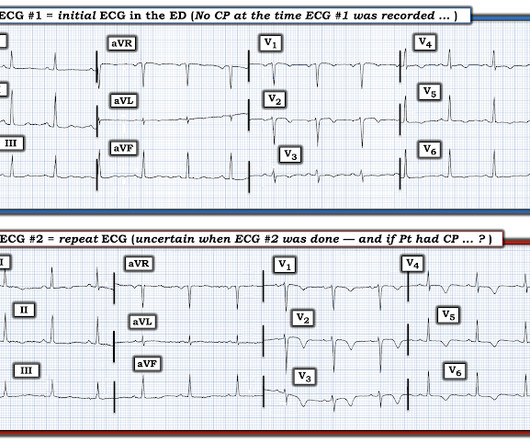
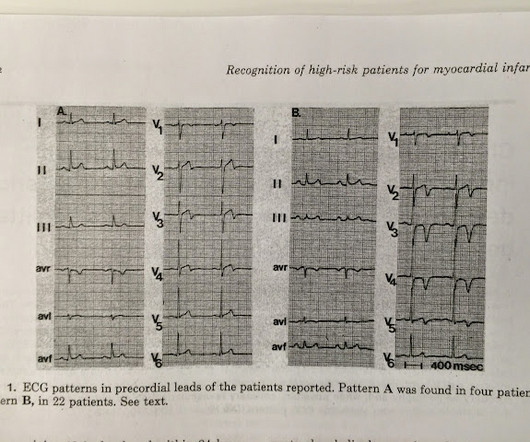
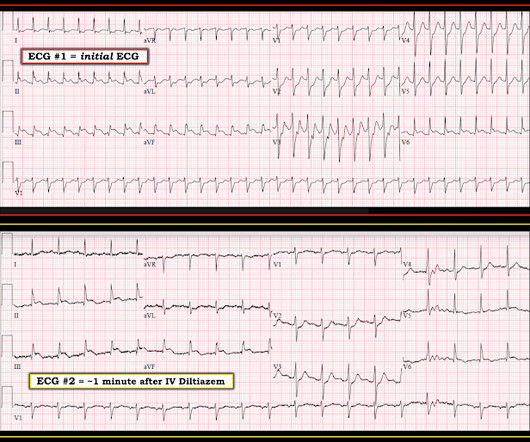
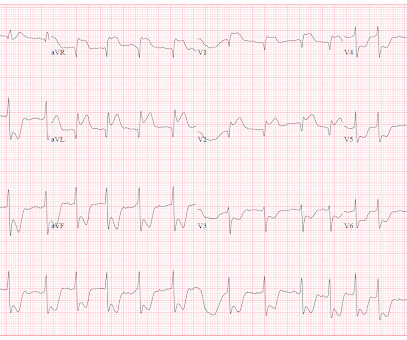
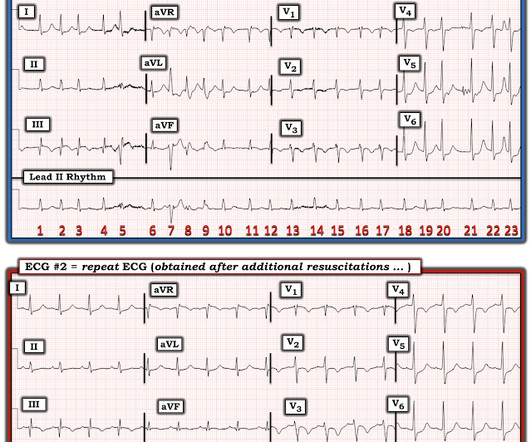
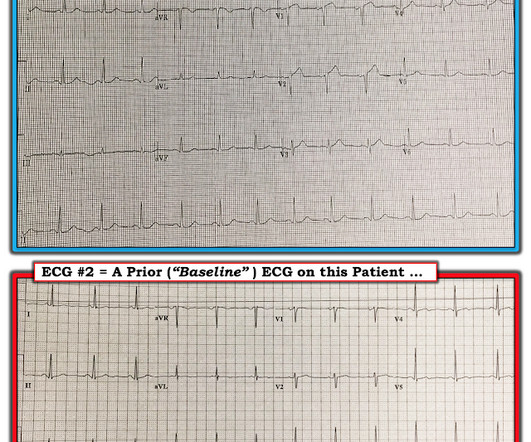
Now as an intern, he is exceptional at EKG interpretation because he was able to learn of the OMI paradigm and importance of pattern recognition before getting poisoned by years of learning STEMI. This is really a transient OMI (or transient STEMI if one uses that terminology and it has diagnostic ST Elevation). He consumed 6 drinks.
















Let's personalize your content