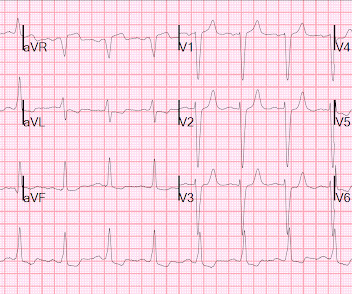
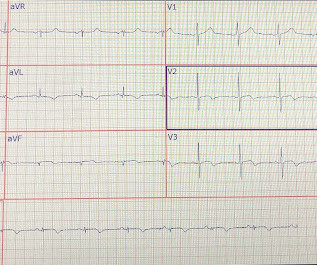
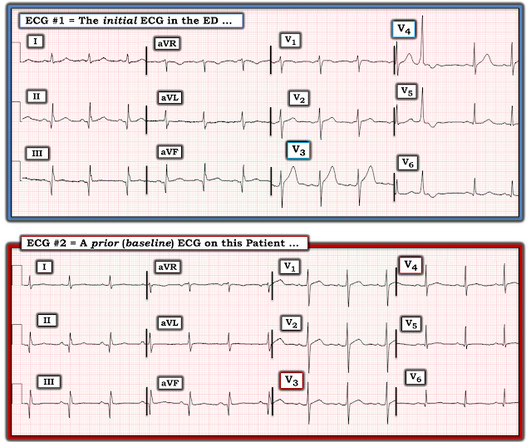
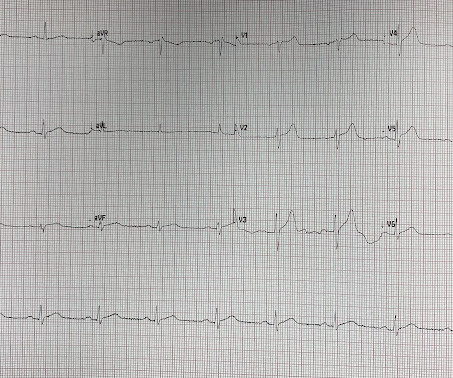
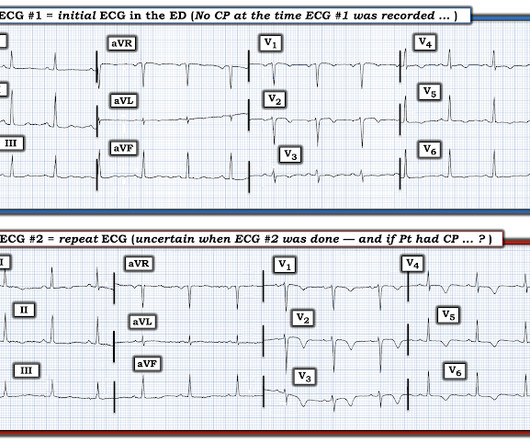
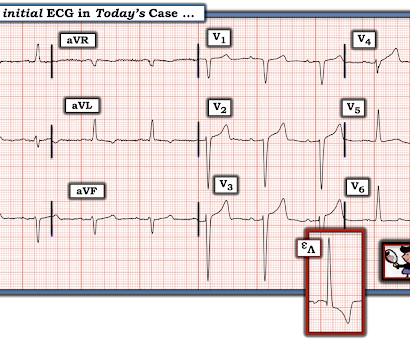
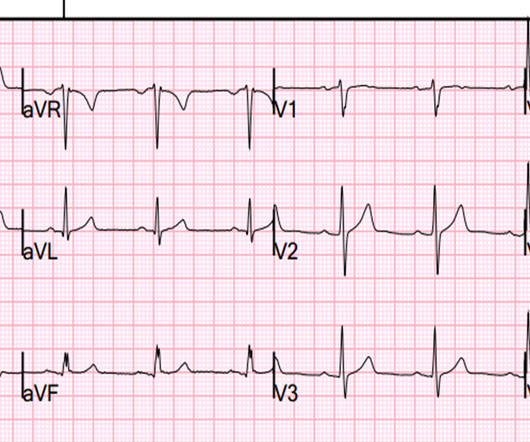
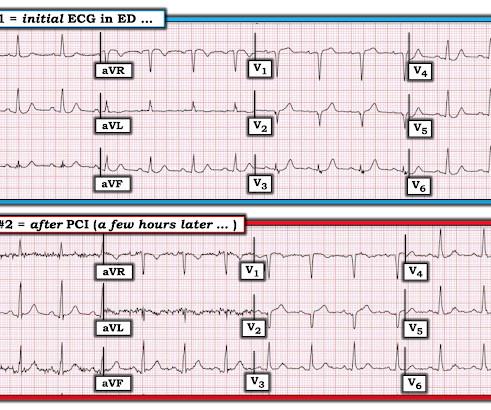
A 70 something female with chest pain (KG- done)
Dr. Smith's ECG Blog
OCTOBER 7, 2022
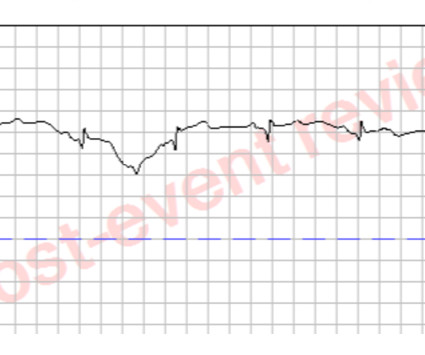
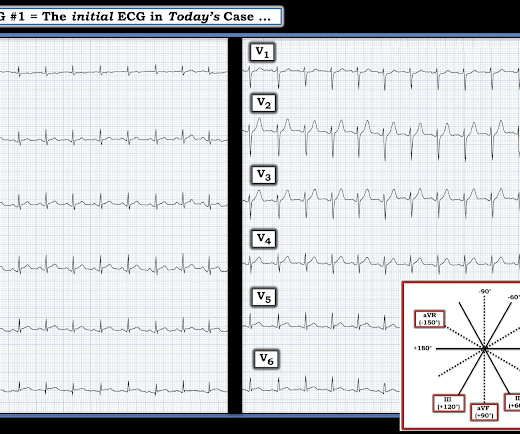
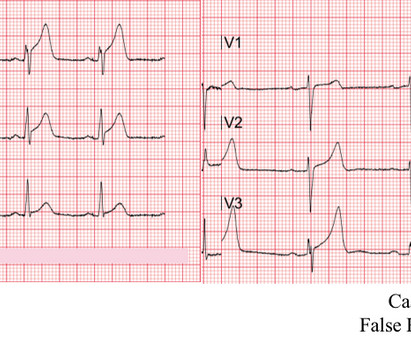
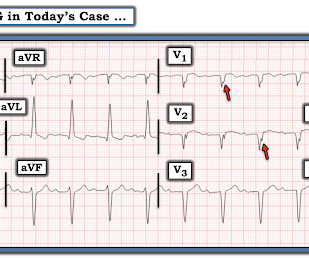
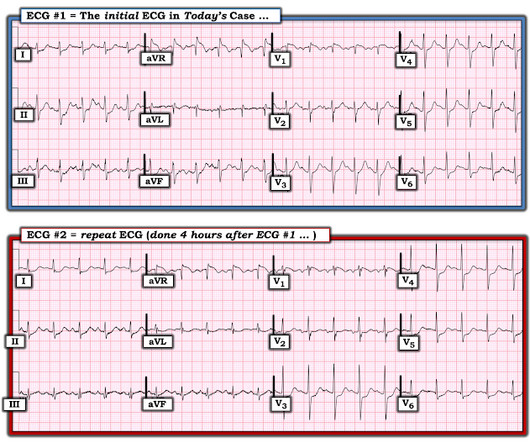
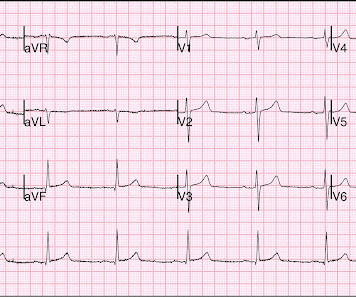
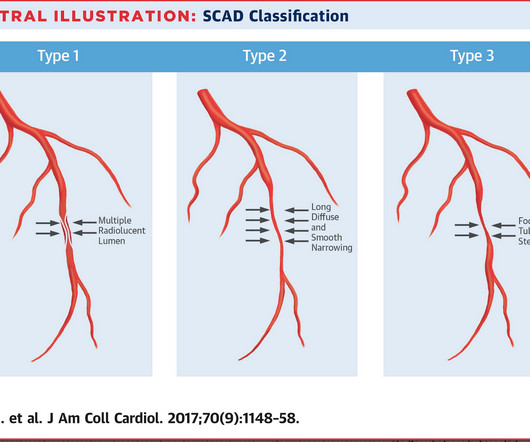
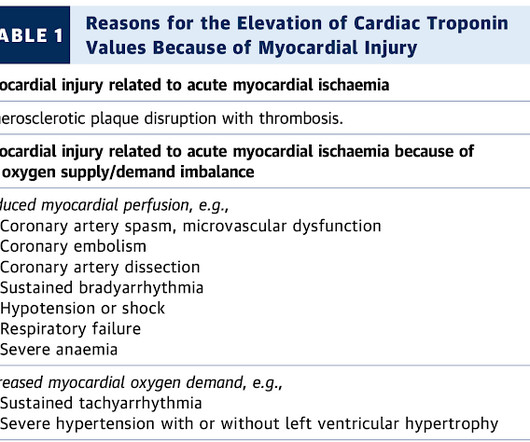
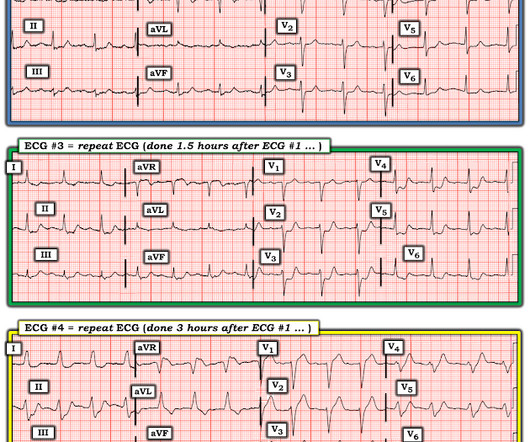
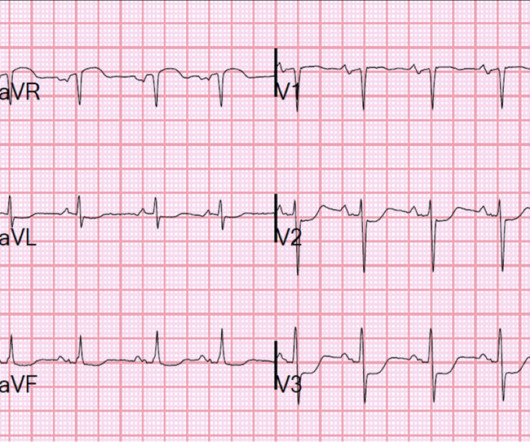
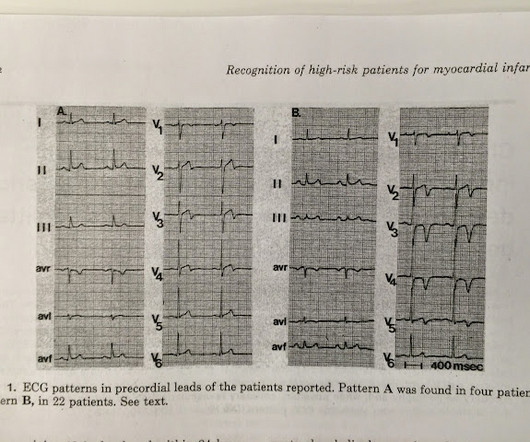
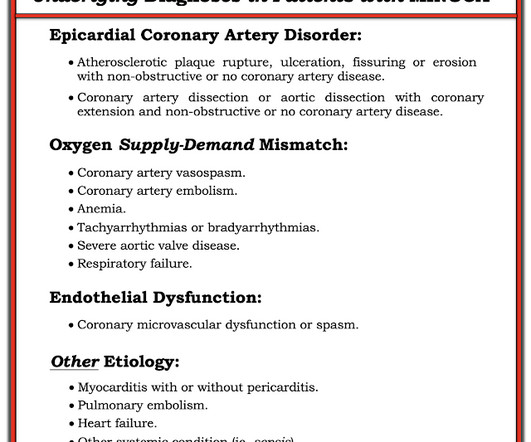
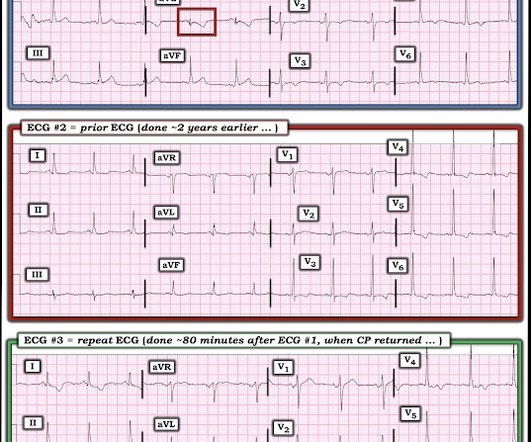
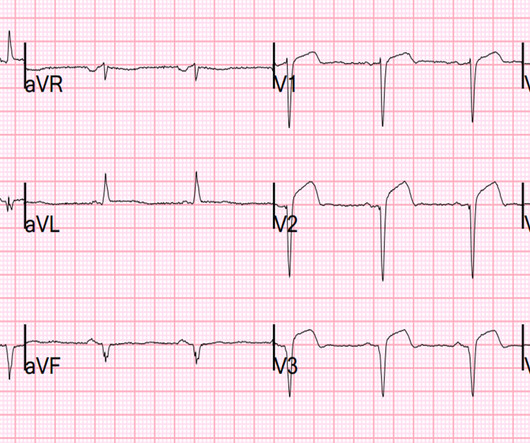
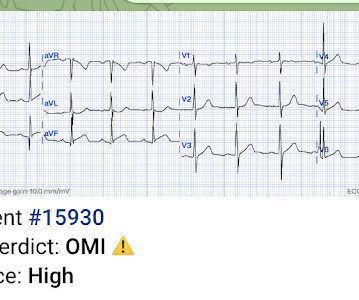
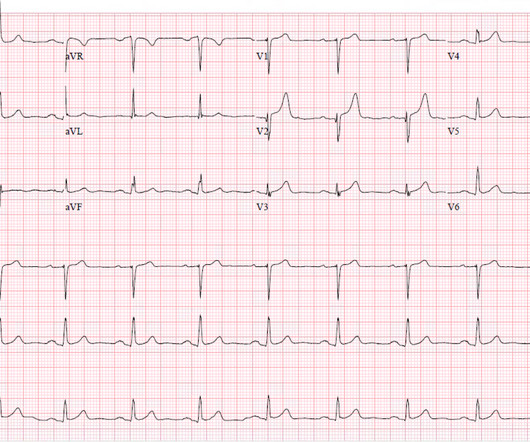
The T wave changes that have occurred are widespread, and not in a typical coronary distribution. Each time the patient underwent cardiac catheterization — and each time, she had patent coronary arteries! We proved this in this article. Note also the loss of R wave amplitude in ECG #2 compared to ECG #1. This patient never had ACS.




















Let's personalize your content