SGEM#462: Spooky Scary Access – IV or IO for OHCA
The Skeptics' Guide to EM
NOVEMBER 30, 2024
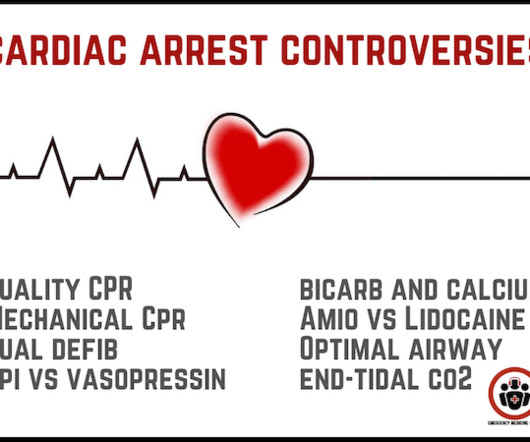
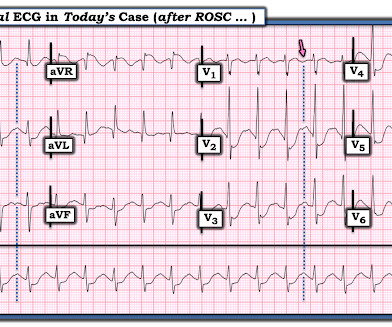
The paramedic is trying to get intravenous (IV) access to give epinephrine per the protocol. Epinephrine has long been a cornerstone in the management of OHCA. Multiple studies have demonstrated how the administration of epinephrine can improve short-term outcomes, such as return of spontaneous circulation (ROSC).





































Let's personalize your content